THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT
30 years old male occupation Working as farmer present to our casualty at 9:15 AM on 13/2/2022 with the chief complaint of dyspnoea since 2 hours and and nausea since 2 hours
HOPI :
Patient is the father of two girls is an alcoholic since past 5 to 6 years with a intake of 90 to 180 ML of whiskey every day .
yesterday night he consumed 90 ML of whiskey following which the patient complained of generalised weakness and two episodes of loose stools .
At 4 AM in the morning patient was hungry so he was given milk when he was in supine position by his attender (mother) Following which the patient started to complain of nausea and he become tachypneic
H/o Intake of herbal medication for one day For alcohol dependence syndrome
Past history :
Not a known case of DM, HTN,TB,epilepsy, CAD, CVA.
Personal history :
Diet : mixed
Appetite : normal
Bowel and bladder moments : regular
Habits/addictions : he Is alcoholic since six years daily intake of whiskey 90 to 180 ML per day.
He chews tobacco one pack for day.
Family history :
No significant family history
Genral examination :
Patient is conscious, coherent , cooperative
No signs of pallor , ictreus, clubbing , Sinuses lymphadenopathy , pedal edema.
Vitals :
Temp :
Bp : 190/90 MMHG
Pr : 120 bpm
Rr : 40 cpm
Spo2 : 60% at ra
Grbs : 210mg%
Systemic examination :
Cardiovascular system : s1 , s2 heard , no murmur
Respiratory system : b/L respiratory crepts in all lung fields.
Per abdomen : soft , non-tender , no organomegaly.
INVESTIGATIONS:
HEMOGRAM:
HB: 17.9
TLC: 4,000
N/L/E/M/B: 85/10/01/04/00
PCV: 53.4
MCV: 90.1
MCH: 30.2
MCHC:33.5
RBC:5.93
PT:2.06
RDW-CV :12.8
RDW-SD: 42.5
PS: NC/NC
RFT:
BLOOD UREA : 21mg/dl
SERUM CREATININE: 0.8 mg/dl
SERUM ELECTROLYTES:
Ca : 9.6
Na+ : 144
K+: 4.0
Cl-: 100
LFT
TB: 1.44
DB: 0.65
SGOT:40
SGOT:15
ALP: 169
TP:7.3
ALBUMIN:3.6
A/G: 1.36
Rbs : 125
Serum osmolality : 302.4
Serology : negative
Complete urine examination :
Albumin : 3+
Sugar : 2+
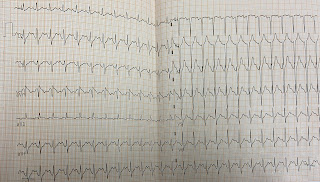
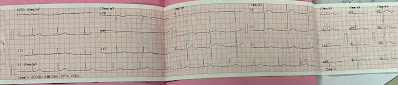
Ecg :
Cxr :
|
|
On admission (13/2/22) |
Post intubation |
14/2/22(8am) |
14(4pm) |
14(11pm) |
15/2/22 , re-intubation (8pm) |
15(9pm) |
15(11pm) |
|
PH |
7.13 |
7.23 |
7.34 |
7.36 |
7.44 |
7.19 |
7.2 |
7.36 |
|
Pco2 |
61.7mmhg |
48.5mmhg |
37.5mmhg |
41.7mmhg |
37.5mmhg |
76.6mmhg |
52.4mmhg |
45.2mmhg |
|
Po2 |
87.5mmhg |
250.7mmhg |
101.5mmhg |
57.7mmhg |
176.5mmhg |
46mmhg |
137mmhg |
75.6mmhg |
|
Hco3 |
19.0mmol/l |
20mmol/l |
20.4mmol/l |
22.3mmol/l |
21.0mmol/l |
28.7mmol/l |
24.5mmol/l |
25.1mmol/l |
|
So2 |
87.4% |
99.3% |
85.3% |
86.5% |
97.3% |
63.8% |
97.1% |
92.4% |
|
|
16/2/22(2am) |
16/2/22(6am) |
16(7.30am) |
16(6pm) |
16(10pm) |
17(2am) |
17(6am) |
17(3pm) |
|
PH |
7.27 |
7.19 |
7.31 |
7.43 |
7.36 |
7.43 |
7.39 |
7.36 |
|
Pco2 |
45.1mmhg |
74.9mmhg |
52.9mmhg |
44.3mmhg |
38.5mmhg |
45.6mmhg |
44.2mmhg |
51.9mmhg |
|
Po2 |
118mmhg |
120mmhg |
140mmhg |
226.4mmhg |
154mmhg |
140.7mmhg |
116mmhg |
121mmhg |
|
Hco3 |
25.9mmol/l |
28.1mmol/l |
25.9mmol/l |
28mmol/l |
22.9mmol/l |
30.2mmol/l |
26.2mmol/l |
31.3mmol/l |
|
So2 |
97.4% |
96.1% |
97.4% |
85.6% |
96.5% |
87.3% |
97.1% |
97.3% |
|
|
17(1.20pm) |
17(4.00pm) |
17(10.15pm) |
18(6.45am) |
18(2.45pm) |
18(7.40pm) |
19(1.45pm) At 3am (self extubated) |
20(12.15am) |
20(6.15am) |
|
PH |
7.39 |
7.43 |
7.51 |
7.44 |
7.23 |
7.39 |
7.48 |
7.42 |
7.45 |
|
Pco2 |
51.9mmhg |
43.3mmhg |
12.9mmhg |
45.4mmhg |
72.6mmhg |
52.8mmhg |
48.0mmhg |
51.5mmhg |
49.1mmhg |
|
Po2 |
121mmhg |
116mmhg |
220mmhg |
69.0mmhg |
110mmhg |
98.6mmhg |
67.8mmhg |
90.8mmhg |
147mmhg |
|
Hco3 |
31.3mmol/l |
28.5mmol/l |
10.3mmol/l |
30.7mmol/l |
29.6mmol/l |
31.4mmol/l |
35.0mmol/l |
32.8mmol/l |
30.2mmol/l |
|
So2 |
97.2% |
98.5% |
96.2% |
90.7% |
95.0% |
95.7% |
91.9% |
95.0% |
97.4% |
|
|
21(12am) |
21(6am) |
|
PH |
7.41 |
7.40 |
|
Pco2 |
34.8 |
37.7 |
|
Po2 |
108 |
91.2 |
|
Hco3 |
21.9 |
23.1 |
|
So2 |
96.1 |
95.0 |
|
|